For more than 20 years, professional journals have speculated on how to retain radiologists across healthcare settings including private practices, academic medical centers, and community hospitals. They knew increasing retirements from an aging workforce would eventually take its toll, so would increasing rates of workplace dissatisfaction. But no one could foresee the havoc wrought by the COVID pandemic.
Add high rates of burnout, competition for compensation, crushing workloads, and you have the perfect storm for radiologists to shop, and leave the practice. To survive and keep talented staff, practices must make retention part of recruitment. It’s not a new idea.
In 2004, the Journal of Medical Practice Management1 published an article urging practices to consider retention as an extension of the recruitment effort. Fast forward to the present day and statistics show that retention isn’t just a good strategy – it’s the only strategy to keep radiologists.
The 2022 Review of Physician and Advanced Practitioner Recruiting Incentives2 shows that radiology is the third most requested specialty, behind nurse practitioners and family medicine physicians. There’s plenty of demand and not enough professionals to go around. Unfilled job openings on the American College of Radiology job board3 are climbing to new heights. That market competition puts radiologists in the driver’s seat and requires that practices find a way to retain good people.

It’s actually not difficult to retain talented radiologists, it’s a matter of dedicating resources to support the strategy. If a practice can address these four issues, there is a good chance it will lead to more successful retention.
Money always talks, and today it is one of the main reasons why radiologists are on the move. The main culprit is the fact that RVUs are increasingly central to compensation. However, when the RVU/incentive balance is out of whack, radiologists know it, and they move on to a more favorable financial environment.
Practices need to make sure that success is possible and the RVU system will truly incentivize, not penalize, radiologists.
A recent Medscape survey4 shows that 54% of radiologists report burnout, many of them saying it is “pervasive and persistent”. Physicians regularly identify the top factors as:
Nearly half the physicians surveyed (45%) said that increased compensation and more manageable work schedule would help alleviate burnout. It is also important that administration should practice continual communication and transparency to improve radiologist satisfaction. Practices can also access the American College of Radiology Radiology Well-Being Program to assist with long-term stress.
Radiologists want to know they are valued. That means making sure they have the modern equipment and effective technology they need to do their job. Transparency is essential in this area. Administration must communicate with the radiology team:
Radiologists want support. Practices should provide support teams to relieve radiologists of administrative burdens so they can handle the demands of increasing workloads.
Another factor to creating a positive work environment is to give radiologists a sense of control over their work, and the opportunity to provide input.
This is an area where teleradiology can play a productive role.The ability to work remotely improves work/life balance and reduces stress, including burnout. Implementing the technology requires only a high-speed, reliable internet connection. The radiologist can work from home and avoid lengthy commutes.
As a result, it is easier to fill call schedules and off shifts. Radiologists are less resistant to filling those shifts because it doesn’t mean rushing to the hospital for emergency imaging, it can be done from home. That can be the tipping point for retaining talented professionals.
Radiologists want more education throughout their career. They want increased knowledge in subspecialties. This is especially important for mid-career radiologists who want training to feel they are valued by the organization. An article in the RSNA Daily Bulletin5 suggests encouraging mid-career radiologists with training and mentors so they don’t feel “stuck” in their career.
Retention means supporting radiologists with strategies that make them feel valued. Most likely the pipeline of available talent isn’t going to improve any time soon. The market is dynamic and these professionals are going to continue to shop for higher compensation and better work environments.
To retain staff, practices must make sure they create and offer that desirable environment. The alternative is not enough staff to provide high quality patient care. And that impacts the bottom line, every time.
Join Daniel Arnold for a conversation with Dr. Francis Deng, neuroradiologist and assistant professor at Hopkins Radiology. Dr. Deng shares his journey on how he came to neuroradiology, and how his research and teaching experiences helped shape his career.
Daniel and Dr. Deng also explore the impact of the National Resident Matching Program on medical education, while discussing the record-breaking radiology match statistics, and the driving forces behind radiology’s resurgence.

Additionally, Dr. Deng discusses AI in radiology education and its potential benefits, while sharing his thoughts on the challenges and opportunities facing the radiology job market.
If you are interested in learning from more leaders in the radiology industry, tune in to the rest of our episodes on the Radiology Report.
You can also listen to the episode on our Youtube channel.
Medscape’s report on physician burnout and depression, ‘I Cry but No One Cares’: Physician Burnout & Depression Report 2023, paints a desperate picture of the emotional status of physicians in nearly all specialties and builds on last year’s findings on radiologist burnout. It remains a crisis that threatens the profession and the statistics paint a picture of urgency.
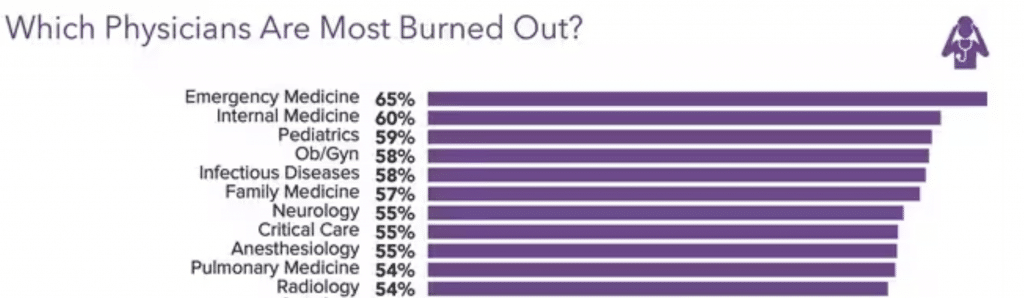
Emergency Medicine physicians have the highest reported rate of burnout at 65 percent, which is striking because just five years ago only 45% of ER doctors reported burnout1. Radiologists round out the top ten specialties, with 54% reporting burnout, an increase over last year, when the survey showed that 49% of radiologists experienced burnout2. The other specialties in the top ten include:
These feelings aren’t new. Nearly two-thirds of the respondents say they have been burned out for 13 months or more and the feelings are “pervasive and persistent”3. Many more female radiologists (65%) experience these feelings compared to 44% of males4. Burnout affects more than just work life; two-thirds of radiologists (67%) say burnout negatively affects their personal relationships5.
We know that in order to maintain quality of care and patient safety we must protect the physical, mental, and emotional health of providers, which begs the question: how are these high rates of burnout allowed to be the status quo?
Radiologists and other physician identify the same top four causes for their burnout6:
Providers also believe there are other contributing factors, namely7:
Taken together, it’s a picture of providers who feel burned out, underpaid, and micromanaged with cumbersome technology and rude patients. It’s a perfect storm that threatens the availability of providers just when the population is aging and needing more care.
Burnout significantly impacts performance and long term career sustainability. Depression impacts daily life and that’s an important distinction. Sixty-seven (67%) percent of respondents report feeling down, blue, or sad, (colloquial depression), and one quarter (¼) of physicians and radiologists report clinical depression, (depression that lasts some time and is not caused by a normal grief event or medical condition)8.
Burnout is named as the leading cause of depression by 64 percent of respondents.
Nearly half of physicians (47%) have not sought professional help to reduce burnout, but would consider it9. Thirty-nine percent said they have not sought help and will not consider it and 13% have sought help10.
The taboo of depression and admitting it exists looms large for providers who say they can’t seek help because “depression says something negative about me” (51%)11. Forty-two percent (42%) say they worry people will think less of their professional abilities and 41% “fear” that the medical board/employer will find out12. Providers express great skepticism and mistrust of administration and colleagues saying; “Our medical board does not help doctors and nurses; they only punish and humiliate,” and “I don’t trust doctors to keep it to themselves”13.
A smaller percentage of radiologists say they treat themselves for depression through meditation (26%), reducing work hours (21%) or speaking with administration about productivity pressure (13%)14.
Fifty-one percent (51%) of physicians and 61% of radiologists said burnout does not affect their patient relationships15. However, there are other areas where burnout is seeping in around the edges, and in a negative way16.*
*(Percentages do not add up to 100% because respondents could make multiple choices.)
It’s imperative that healthcare organizations of all sizes take these skyrocketing rates of burnout seriously. It has long lasting effects that can impact patient care, quality and safety, and cause radiologists to leave a field that is already suffering from severe staff shortages.
Protecting the health and wellness of providers is not a luxury, it is a requirement. It behooves healthcare organizations to take stock of work hours, productivity requirements, onerous EHR documentation, and staffing shortages.
If we are to move into the future with a highly skilled workforce that delivers the best care to patients, then employers and partners must do everything in their power to find innovative solutions that will protect the mental, physical, and emotional health of essential radiologists and clinical providers.
References
1-16: ‘I Cry but No One Cares’: Physician Burnout & Depression Report 2023 (medscape.com) Leslie Kane, MA, Executive Director, Medscape Business of Medicine, January 27, 2023