For more than 20 years, professional journals have speculated on how to retain radiologists across healthcare settings including private practices, academic medical centers, and community hospitals. They knew increasing retirements from an aging workforce would eventually take its toll, so would increasing rates of workplace dissatisfaction. But no one could foresee the havoc wrought by the COVID pandemic.
Add high rates of burnout, competition for compensation, crushing workloads, and you have the perfect storm for radiologists to shop, and leave the practice. To survive and keep talented staff, practices must make retention part of recruitment. It’s not a new idea.
In 2004, the Journal of Medical Practice Management1 published an article urging practices to consider retention as an extension of the recruitment effort. Fast forward to the present day and statistics show that retention isn’t just a good strategy – it’s the only strategy to keep radiologists.
The 2022 Review of Physician and Advanced Practitioner Recruiting Incentives2 shows that radiology is the third most requested specialty, behind nurse practitioners and family medicine physicians. There’s plenty of demand and not enough professionals to go around. Unfilled job openings on the American College of Radiology job board3 are climbing to new heights. That market competition puts radiologists in the driver’s seat and requires that practices find a way to retain good people.

It’s actually not difficult to retain talented radiologists, it’s a matter of dedicating resources to support the strategy. If a practice can address these four issues, there is a good chance it will lead to more successful retention.
Money always talks, and today it is one of the main reasons why radiologists are on the move. The main culprit is the fact that RVUs are increasingly central to compensation. However, when the RVU/incentive balance is out of whack, radiologists know it, and they move on to a more favorable financial environment.
Practices need to make sure that success is possible and the RVU system will truly incentivize, not penalize, radiologists.
A recent Medscape survey4 shows that 54% of radiologists report burnout, many of them saying it is “pervasive and persistent”. Physicians regularly identify the top factors as:
Nearly half the physicians surveyed (45%) said that increased compensation and more manageable work schedule would help alleviate burnout. It is also important that administration should practice continual communication and transparency to improve radiologist satisfaction. Practices can also access the American College of Radiology Radiology Well-Being Program to assist with long-term stress.
Radiologists want to know they are valued. That means making sure they have the modern equipment and effective technology they need to do their job. Transparency is essential in this area. Administration must communicate with the radiology team:
Radiologists want support. Practices should provide support teams to relieve radiologists of administrative burdens so they can handle the demands of increasing workloads.
Another factor to creating a positive work environment is to give radiologists a sense of control over their work, and the opportunity to provide input.
This is an area where teleradiology can play a productive role.The ability to work remotely improves work/life balance and reduces stress, including burnout. Implementing the technology requires only a high-speed, reliable internet connection. The radiologist can work from home and avoid lengthy commutes.
As a result, it is easier to fill call schedules and off shifts. Radiologists are less resistant to filling those shifts because it doesn’t mean rushing to the hospital for emergency imaging, it can be done from home. That can be the tipping point for retaining talented professionals.
Radiologists want more education throughout their career. They want increased knowledge in subspecialties. This is especially important for mid-career radiologists who want training to feel they are valued by the organization. An article in the RSNA Daily Bulletin5 suggests encouraging mid-career radiologists with training and mentors so they don’t feel “stuck” in their career.
Retention means supporting radiologists with strategies that make them feel valued. Most likely the pipeline of available talent isn’t going to improve any time soon. The market is dynamic and these professionals are going to continue to shop for higher compensation and better work environments.
To retain staff, practices must make sure they create and offer that desirable environment. The alternative is not enough staff to provide high quality patient care. And that impacts the bottom line, every time.
Medality CEO and Co-Founder, Daniel Arnold, and VP of Educational Strategy and Operations, Deanna M. Heier, PhD recently chatted with The Imaging Wire to discuss how practices can take advantage of growth opportunities, despite the radiology labor shortage, by helping their radiologists upskill in critical areas.
Brian Casey: Hello and welcome to the Imaging Wire Show. My name is Brian Casey and I’m Managing Editor of the Imaging Wire. We’ve got a great episode for you today. Our topic is Practice Growth Opportunities: Overcoming the Radiology Labor Shortage and our guests are Daniel Arnold, CEO and Co-founder of online education company Medality and Deanna Heier, PhD, Medality’s Vice President of Educational Strategy and Operations.
Dan and Deanna, thanks for being with us today.
Daniel Arnold: Thanks for having us on the show, Brian. I’ve been an avid reader of yours since I started in the industry and a big fan of The Imaging Wire and really grateful to be here.
Brian Casey: Awesome, it’s great to have you. Now, most folks might know you from when Medality was called MRI Online. Dan, can you introduce yourself and tell us a little bit about the rebranding?
Daniel Arnold: Well, first of all, just the fact that you say most folks may know you is humbling. I remember when I first started the company, I would sit alone in my apartment late at night hitting refresh on the website to see if anyone visited us and we’ve come a long way since then. We started out with just one course in MSK Knee MRI, and as it will quickly become apparent throughout this call, I’m not a radiologist by training, my background is in technology, so I thought, we’ve got a course on MRI, we’ll call it MRI online.
We gained a lot of traction really quickly and then customers started asking us “do you have courses in CT, do you have courses in Mammo? You know, we have a lot we need to learn.” And so I quickly learned that we needed to broaden the horizons of our training. And so we’ve since gone on to expand our offering to cover all modalities and all subspecialties of radiology and over time, we’ll enter new medical specialties as well.
And so the name Medality actually has a lot of meaning for us. First of all, modality has a lot of meaning in imaging. And we teach across all modalities. Modality also has meaning within education. Some people are visual learners, some are interactive learners, some are auditory learners. And so we take people’s multiple modalities of learning, multiple modalities of health care and medicine and brought that all together for our new name Medality.
Brian Casey: Awesome. And it’s been great to see you guys evolve. Deanne, can you tell us a little bit about your background?
Deanna Heier: Sure. So I come from a background of scientific research, and I’ve been working in medical education for the last 20 years, which is always hard to think about how long.
But I’ve really come to love this field. And when I met Daniel and saw what Medality was doing to disrupt traditional CME, I was hooked. You know, basically being able to take what we’ve been doing online for education to a new level with a more interactive and simulation based training model that we know has better impacts was what really brought me here.
And I had never worked in radiology before. And as I learn the field of radiology, I just have seen what a great impact that this education can have. So that’s why I’m here and I do it…I’m really just passionate about working in a field where we can really make some strides and have a great impact on patient care.
Brian Casey: Great. Now, if we can start kind of at a high level, can we talk a little bit about the traditional model for radiologist education and training?
Daniel Arnold: Sure. So my background is actually in technology. I started out my career at Google where I was building new online products, one of which was in the online education space. And I was building up partnerships with companies like Khan Academy and Coursera and Masterclass.
If we’re using things like microlearning, short 2 to 4 minute interactive videos, paired with simulation training to really disrupt the way that people learn. That’s sort of it. I got my MBA. I wanted to start a business and my wife Tayler was going into radiology for residency. In med school, she had relied on many of these online education platforms to learn. She’s actually never been a very good reader. She always struggled to get through textbooks and journals. And so these online education applications that she used throughout med school really transformed her ability to get through this period. And then when she got to residency, she matched at Penn. She was all excited and the first thing they emailed her was “here’s your prerequisites list” and on the list was Dave Yousem’s textbook called Neuro Requisites and it was 300 pages. And I looked at her and we started laughing. “Oh my goodness, right? Residency is going to be hard. Is this all there is in radiology residency? There’s no Khan Academy for radiology?”
And so your traditional model of teaching radiology is an apprentice model. And what’s great about radiology is it’s a resident, it’s a trainee sitting side by side with an attending, working through an actual patient case. And that model is proven to be the best way to learn. But then all the learning that happens outside of that, outside of that at the workstation learning has to happen on your own. And so it used to be, you know, you go to the hospital during the day and then at night you go to the library and read for 4 hours.
And that model just doesn’t really fit with today’s modern resident. They’re busy. My wife and I…we had three kids during residency, so having a four hour stretch to go sit at the library wasn’t a reality. And we thought there must be a better way. And so that’s one way education has changed. We’re trying to move away from analog training models to digital training models.
And one of the other big trends is that over the last 20 years, there’s been a really increasing focus on subspecialization in radiology. It used to be you do a general radiology training or maybe one fellowship in a broad area like MRI that you would practice across multiple subspecialty areas. Since the field’s gotten much more subspecialized, over 98% of people in the United States subspecialize, which is on the whole, very good for patient care.
As a result, I think we’re a lot deeper and more knowledgeable, more sophisticated at treating diseases in areas like pediatrics and neuroimaging and the like. But the realities of practice today is that people have to practice outside of just their core subspecialty. We’re going to talk a lot about the data in our report later about what those trends look like.
But so, as a result, your education, you can leave training and not have as broad a skill set as you might have had ten or 15 years ago. And so then when you leave your academic training setting and get into the real world, which is where we’re focused, our business is focused on helping real world clinicians practice more effectively. You find that you have some training gaps, we’ll get into that a little bit.
Brian Casey: Yeah. So you mentioned this apprentice model of an apprentice sitting next to a mentor at a workstation. And I’m just sitting here going like, how did that work during COVID? You know, because you’re not allowed to be in a room with anybody. So did that have a big impact on your company and your evolution?
Daniel Arnold: It did. So when we first started the company, I thought, “okay, we’re going to build this world class studio. We’re going to fly radiologists in to build courses.” And we opened the studio in February 2020. It became very apparent very quickly that no one’s going to be flying to Cincinnati to build our courses, which is where we’re from.
But then the other thing that became really apparent is that residency programs were going to shut down and people weren’t going to be able to do their in-person learning. And, you know, we started reading up on this little company called Zoom. We go…“hey, you know, I think we could do a lecture conference.” We started a lecture series and we invited five of the top radiologists we knew: Neuro Radiologists, Body Radiologists to do a lecture, and each one got attended by over a thousand people that first week because all of the residency programs had shut down and they couldn’t get their training. And so we actually quickly became an integral tool, not just for residency programs that we found though, you know, we thought, okay, this would be great for residency programs, is that actually practicing radiologists would really value this content as well because for them, they couldn’t go to their conferences anymore. So you couldn’t go to Park City for your head and neck conference. You couldn’t go to Hawaii anymore either. And so the audience quickly brought in, which helped us come into focus.
Brian Casey: Now, Deanna, can you talk a little bit about some of the services that Medality offers right now that address some of these training issues that Dan has been talking about?
Deanna Heier: Yeah, sure. So Daniel touched on it a little bit. But you know why we’re different and, what attracted me here is, well, it’s really that learning model that draws you in. So it’s moved away from the more passive style of learning. You know, watching endless YouTube videos isn’t going to get you there. It can start you off and give you a foundation.
But what our model really does, the service we offer is a microlearning simulation based model. And so what that means, what that breaks down to is microlearning. You know, it’s accessible, it’s something you can do, which is just 5 minutes here or 5 minutes there. We hear from a lot of radiologists actually that tell us different places that they learn alongside us, whether it’s watching the Super Bowl or on their Pelotons and things. So it’s really trying to incorporate your professional development into your every day because they’re trying to make every minute work.
And the simulation based side of it is where the impact really happens. And what we do is we put the real DICOM images that radiologists are looking at day to day. So just like if you were at your workstation, you’re going to be able to scroll through that image and watch somebody like Dr. David Yousem scroll through that same brain CT and you’ll be able to see the search patterns that he’s using. How does he evaluate that lesion? How does he move forward to interpret and report on that lesion and really help them kind of hone those skills, make sure you’re not missing and doing it really efficiently because once you know the fundamentals, it’s more about how do you now deal with the volumes that you’re facing day to day, right?
So how do you get really efficient at what you’re doing day to day? So when you see that case come up in your workstation, you’ve seen it before and you know what to do and you know how to handle it.
Brain Casey: It almost sounds like you’re sort of sitting there next to Dr. Yousem while they’re going through a case.
Deanne Heier: It’s a great model. So, I mean, think about it. The way we work today, you’ve got more than one screen in front of you, right? Especially if you’re at your workstation, so you literally have your scan that you’re looking at on one and you have Dr. Yousem working through that same scan on your other screen.
And it’s just like you were back in residency, you know who’s going to those good ol’ days. Where you were able to just be there and learn and soak it all in. And so we have hours and hours of experts just scrolling through cases on our site. And so really go back to those days and reinforce some of those cases you haven’t seen in a while and just build your confidence.
Brian Casey: And you can do it all in your pajamas.
Deanne Heier: Yup. Some of them do. Some people share that.
Brian Casey: Yeah. So you recently published a report on radiologist education and training. Can you talk a little bit about the report and what some of the findings are in there? And then we’re going to look at some data in a second.
Deanne Heier: Yeah, sure. So in working through all of these cases…we’ve been working with a lot of radiologists, a lot of private practices around the world, and we realized that we have a lot of needs assessment data.
So our approach to learning is that we really only develop courses that radiologists need for their day to day practice. So we do needs assessments that tell us what areas radiologists are confident in or less confident in, what are they currently reading, what do they want to be reading in and what are those barriers? And a lot of times it’s just training or exposure or lack of exposure to cases.
And so we found we were collecting quite a lot of data. Last year, we collected over 2,700 radiologists who were working with us, and so we wanted to share it out. We were seeing some interesting trends and we wanted to be able to share some of those gaps and opportunities that we were seeing in the data. And that’s how the report came to be.
Brian Casey: All right. So we actually do have some of the data from that survey. So let’s take a quick look at it. And this is from a survey of 2,700 radiologists, correct?
Deanne Heier: That’s right, yeah, a little over 2,700. You know, we asked them some pretty basic questions just about what their day to day is. And one of those questions was “What subspecialties do you currently read in your daily practice?” And 40% reported that they read across all of the subspecialties so we had a list of them that they can pick from and they said, “no, I read across all of these on any given day I might see a scan in any of these subspecialties.” And then the other 60%, you can see the results from those here.
The highest reads were happening in Neuroradiology and MSK then Body so both GI and GU. So those weren’t maybe too surprising but what did strike us is outside of everybody’s reading general radiology, people are still reading 4 to 5 subspecialties in their day to day practice. And that really surprised us. You know, Daniel mentioned that training a lot of times it’s very focused on some specialization. And so the fact that the reality is that they’re not only reading in their subspecialty areas, they’re actually reading across many subspecialties.
Daniel Arnold: And if you think about Brian, the pace of change in radiology, I think one of the reasons people love radiology is the fast pace of change. If you look at areas like Stroke Imaging, Breast Imaging and Prostate Imaging to take three, the pace at which those have changed in just the past five years from no Tomo adoption to Tomo being the standard of care. And from stroke protocols completely being reinvented.
If you’re a general radiologist or you’re an MSK radiologist, but then you’re practicing outside those areas. That’s a lot of information to stay up to date on, to be able to provide high quality care to your patients. And so this helped us realize just how broad the need is within a large radiology practice. You’re going to have multiple training needs just for each radiologist in your group.
Brian Casey: Yeah, and a couple of things are at the bottom there, cardiac and nuclear kind of low percentages. And we’re going to run into that in a second. So what are we looking at here now?
Deanne Heier: So another question we asked is just how confident they are when they’re reading in those different subspecialties. And so the data you’re seeing here are the subset that are reading in each of these subspecialties. So we’ve taken out anybody who’s not currently reading in the subspecialty and just ask them how confident they feel when the studies come through. And so you can see here most people are confident, but quite a large percentage are only somewhat confident, right?
So there’s inevitably cases that come up that you’re concerned about. You’re just not sure that you’ve seen that case before. You know, I think radiologists as a group tend to be a more humble medical specialty. So there’s probably some of that in here. But you see the trend. The trend is that less than half are very confident when they’re reading in their given subspecialty that they’re working in on that day.
Daniel Arnold: I was just going to say, and one of the things to think about is how does confidence impact a radiologist and how does that impact a radiology practice. Patient care is first and foremost, if I’m not confident, I’m not going to provide a good diagnosis. And so now I don’t think this means that a quarter of people are providing bad diagnosis. I think we might be going a little slower. They might maybe not be taking studies on that they might otherwise want to and that causes problems in the practice around turnaround time or just a few people having to take on the most complicated studies, which creates all sorts of challenges within practice. So if you’re wondering, “hey, why are my prostate MRs sitting on the list? Why are my advanced head and neck cancer staging studies staying on the list for a week?” Oh, well, it’s because Dave is out on vacation and the other rads we have in the practice that claim to read neuro, they’re just not confident enough to take that on.
And so trying to understand these areas where radiologists are reading but not as confident as they can be in certain areas can help you plug some pretty targeted holes within your practice that can really improve efficiencies within the group.
Brian Casey: Yeah and on imaging where we reported on a study a few weeks ago on cherry picking from the work list, and this study found that cherry picking actually has pretty serious downstream effects on turnaround times and hospital length of stay and things like that. So, you know, it’s a big issue.
Deanne Heier: There is another interesting thing that came out of the results that we’re seeing here that caught our attention. You keep seeing Cardiac and Nuclear Medicine there at the bottom of the list. And those are two really key fields in imaging right now that we know are high growth areas. And so, the fact that we see not as many radiologists reading in those areas and also the ones that are really aren’t feeling as confident as they’d like to be, those were two core places for us that we saw a great need for education and training.
Brian Casey: Great and I think that feeds into the next slide that we’re going to take a look at right here.
Deanne Heier: Yeah, so this is an interesting question we asked. First, we asked them what are they currently reading in? And you can see the breakout there of current readers. But then we asked the group that was not currently reading in the specialty if they would want to.
And what you see here in the coral color is that particularly in Cardiac, we’d be able to double our workforce capacity in Cardiac by providing training and exposure to more general radiologists who are interested in reading in that specialty area. So we started to see again these needs, which is great because it’s a high growth area where training can really have a great impact.
As we know, the guidelines in Cardiac have changed in recent years and so the volumes are increasing and we need to make sure that our radiologists are ready for those orders as they come in. Nuclear Medicine, another great field where we are about to see a huge change, big transformation…the field of Theranostics. I’m sure you’ll cover that in Imaging Wire as well is one that can revolutionize imaging.
And so having radiologists be ready to be on the forefront of big changes like that is a way that training can really take them to the next level.
Brian Casey: When it comes to Cardiac, do you get the feel from your customers that maybe radiology is starting to maybe clawback a little bit of cardiac imaging from cardiologists?
Daniel Arnold: It’s a great question, Brian. We have a regular ad board meeting filled with subspecialty leaders as well as practice leaders who kind of report from the trenches what’s going on. And what they’re saying is that the cardiologists don’t want it. They don’t want it right now because they’re having their own challenges keeping up and they don’t want the liability and everything else that comes alongside it.
And so they’re starting to win back a little bit of the volumes and what’s made our solution unique and where we’re just so different than anything that’s come before it. What makes Cardiac particularly challenging to learn is that it’s a very different software to interpret. You’re actually doing 3D reconstructions of the blood vessels, you’re flying it through and try and identify plaque and other sorts of issues and so you can’t just read a textbook and figure it out.
So in the past, maybe you could go to a workshop for three days…Some are across the country and you better hope you learned it in those three days, because then you get home and you’re on your own. And then, by the way, the group has some challenging discussions to figure out as well, because it’s a pretty big investment if you want to build up a cardiac CT practice.
So you go “hey, do we want to upgrade our CT equipment? Do we want to add new software capabilities?” Well you have to have a confident reader. If I don’t have a confident reader to bill around to go bill the referring base and it becomes very challenging. You have a little bit of a chicken and the egg problem where groups say, “we would love to take on some more volumes. I don’t know if we have a reader who could really own this thing.” And if you want to just hire a cardiac reader, I mean, good luck. Get in line. As we talked about, this is a big, challenging market to hire in any specialty right now. And so what we’ve done is actually partnered with TeraRecon, the market leader in 3D reconstruction for Cardiac CT.
So you can actually do simulations in the cloud before you even invest in this new technology. And then you have access to all those learning cases. So once you’ve gone through it, you know, you can go back and reference that. We also then pair that with expert readers that give you feedback on your reports and usually submit test reports on actual patient cases where you don’t know the answer.
You get feedback, saying “Daniel, you missed this thing or you got the answer right but you didn’t describe it in a way that’s going to really solve the critical question for the physician. Here’s how you could have improved the sophistication of your report.” So by the end of this fellowship, this mini remote fellowship is what we call them, you have enough confidence to say, I actually think I could help us, take on some of these volumes at our group.
Brian Casey: Awesome. Well, this is great data. Are you guys going to continue doing these reports in the future?
Deanne Heier: That’s our goal. So, we really dug into the data quite a bit. We learned a lot and there’s lots of tidbits you’ll see in the full report, just great needs around MRI education and in these new fields.
But yes, this is an ongoing survey. So every day we’re having hundreds more survey results come in. So we’re looking forward to watching those trends over time and some new data that you’ll see year over year. So first, it was more of the needs assessments, but now we’re really evaluating people’s skills, their proficiency, their accuracy and efficiency at reviewing these cases.
And so I’m excited to see all the data that’s coming out and we’re happy to share with the field.
Brian Casey: So this is really great information. Where can people find more information about this report if they want to dig into it deeper?
Daniel Arnold: Yeah, a few places to come. One is definitely check it out at Medality.com, our website will publish the report.
We also have a podcast ourselves where we’re going to be talking with leaders about the report, different trends that they saw on the radiologyreportpodcast.com and you can find that on my LinkedIn profile. So connect with me if you have thoughts and we love to chat about them with you.
Brian Casey: Perfect. We’ll definitely do that. So as we draw to a close, any advice that you have for radiology practices that might be struggling with education and training issues apart from just going to Medality.com and signing up?
Daniel Arnold: Sure. So I think the real framing of the question is the challenge. I think if you ask the large radiology practice, they might not know they have a training-in-development problem. They’ll say we’ve got a labor shortage problem. They’ll say we don’t have enough trained, you know, we don’t have enough capacity of radiologists. They’ll say we want to grow our practice. We’re winning new contracts. We can’t keep up with the volumes. I don’t think their initial thought is always training. I think they think, “Oh, maybe AI can help. Maybe midlevel providers can help. Maybe we can cut off lower end volumes”, those types of things, but they’re not always thinking about training. And so I think for us, helping folks realize that training their workforce and upskilling their workforce can be a real area of capacity for them is part of what this whole exercise is about.
And I’ll just give an example. We do something called a Remote Fellowship. Through our Remote Fellowship in Neuroradiology we followed a cohort of radiologists, post fellowship, and we found that they are reading 20 additional advanced imaging neuro studies six months after their fellowship. This is on top of their existing workload. So they weren’t taking on these studies before and now they’re finding 20 additional RVUs per week. And you see that in areas like Prostate MRI.
So one of our largest customers is called I-MED Radiology. They have 500 radiologists in Australia. They’re the biggest radiology group in the country and they go “Daniel, we need ten more prostate readers tomorrow because we’re growing our service lines in all these areas.” And so, they’re looking, where a group might initially think about hiring, they’re looking at training within. And then are assessment capabilities, which we’ve shared some of those reporting on. We usually roll those assessments out within a group. And so within a group we can help identify individuals within the practice that might have skills or desire areas for new skills in the areas aligned to your growth. And so, you know, if people take anything away from this, I think it’s to try to think a little bit more about how professional development and investing in your radiologists might lead to areas like increased capacity within your workforce.
Brian Casey: Great. Some great, great parting words. Well, Dan, thanks so much. Deanna, thank you so much for sharing all this amazing information. It’s been great talking to you guys and getting your take on the world of education and training in radiology.
Deanne Heier: Thanks for having us Brian.
Daniel Arnold: Thank you so much for having us. Yeah, this is great.
Brian Casey: All right. Signing off for The Imaging Wire. My name is Brian Casey.
Medscape’s report on physician burnout and depression, ‘I Cry but No One Cares’: Physician Burnout & Depression Report 2023, paints a desperate picture of the emotional status of physicians in nearly all specialties and builds on last year’s findings on radiologist burnout. It remains a crisis that threatens the profession and the statistics paint a picture of urgency.
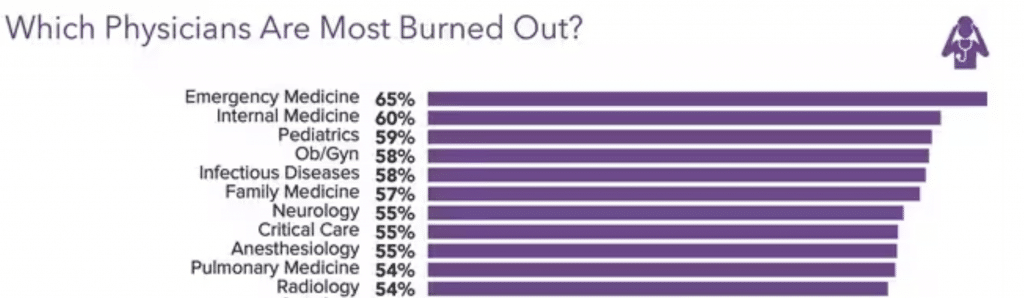
Emergency Medicine physicians have the highest reported rate of burnout at 65 percent, which is striking because just five years ago only 45% of ER doctors reported burnout1. Radiologists round out the top ten specialties, with 54% reporting burnout, an increase over last year, when the survey showed that 49% of radiologists experienced burnout2. The other specialties in the top ten include:
These feelings aren’t new. Nearly two-thirds of the respondents say they have been burned out for 13 months or more and the feelings are “pervasive and persistent”3. Many more female radiologists (65%) experience these feelings compared to 44% of males4. Burnout affects more than just work life; two-thirds of radiologists (67%) say burnout negatively affects their personal relationships5.
We know that in order to maintain quality of care and patient safety we must protect the physical, mental, and emotional health of providers, which begs the question: how are these high rates of burnout allowed to be the status quo?
Radiologists and other physician identify the same top four causes for their burnout6:
Providers also believe there are other contributing factors, namely7:
Taken together, it’s a picture of providers who feel burned out, underpaid, and micromanaged with cumbersome technology and rude patients. It’s a perfect storm that threatens the availability of providers just when the population is aging and needing more care.
Burnout significantly impacts performance and long term career sustainability. Depression impacts daily life and that’s an important distinction. Sixty-seven (67%) percent of respondents report feeling down, blue, or sad, (colloquial depression), and one quarter (¼) of physicians and radiologists report clinical depression, (depression that lasts some time and is not caused by a normal grief event or medical condition)8.
Burnout is named as the leading cause of depression by 64 percent of respondents.
Nearly half of physicians (47%) have not sought professional help to reduce burnout, but would consider it9. Thirty-nine percent said they have not sought help and will not consider it and 13% have sought help10.
The taboo of depression and admitting it exists looms large for providers who say they can’t seek help because “depression says something negative about me” (51%)11. Forty-two percent (42%) say they worry people will think less of their professional abilities and 41% “fear” that the medical board/employer will find out12. Providers express great skepticism and mistrust of administration and colleagues saying; “Our medical board does not help doctors and nurses; they only punish and humiliate,” and “I don’t trust doctors to keep it to themselves”13.
A smaller percentage of radiologists say they treat themselves for depression through meditation (26%), reducing work hours (21%) or speaking with administration about productivity pressure (13%)14.
Fifty-one percent (51%) of physicians and 61% of radiologists said burnout does not affect their patient relationships15. However, there are other areas where burnout is seeping in around the edges, and in a negative way16.*
*(Percentages do not add up to 100% because respondents could make multiple choices.)
It’s imperative that healthcare organizations of all sizes take these skyrocketing rates of burnout seriously. It has long lasting effects that can impact patient care, quality and safety, and cause radiologists to leave a field that is already suffering from severe staff shortages.
Protecting the health and wellness of providers is not a luxury, it is a requirement. It behooves healthcare organizations to take stock of work hours, productivity requirements, onerous EHR documentation, and staffing shortages.
If we are to move into the future with a highly skilled workforce that delivers the best care to patients, then employers and partners must do everything in their power to find innovative solutions that will protect the mental, physical, and emotional health of essential radiologists and clinical providers.
References
1-16: ‘I Cry but No One Cares’: Physician Burnout & Depression Report 2023 (medscape.com) Leslie Kane, MA, Executive Director, Medscape Business of Medicine, January 27, 2023
Hiring talented radiologists is hard. Retaining them is critical.
In a study of annual practice separation rates, researchers found 41% of all radiologists left at least one job within 4 years.[1] And it’s only getting worse.
Fewer radiologists, bigger workloads, and growing demands for imaging make this the most competitive hiring market we’ve ever seen. That’s why it has never been more important to attract and retain radiology talent to your practice.
Give your practice the competitive edge it needs with our 10 tips that can help you overcome hiring challenges, keep your team engaged, and foster growth opportunities:
[1] https://www.neimanhpi.org/press-releases/radiologists-job-changes-trends/#:~:text=Researchers%20found%20that%20over%20the,job%20during%20the%20study%20period.
As a practice leader, it is important to ensure that your radiologists are up-to-date with the latest industry developments and certification requirements. Continuing medical education (CME) is an essential component of maintaining and improving the knowledge, skills, and performance of healthcare providers. Managing and tracking CME hours can be a complex and time-consuming process, particularly when you are responsible for overseeing a large team of radiologists.
Medality is a Practice Development Platform that offers a one-stop-shop for CME for radiologists. With our platform, you can create CME pathways for your radiologists and enroll them in affordable training courses based on their necessary certifications and state requirements. This makes it easy for you to manage your team’s CME certification process and ensures that your radiologists are always up-to-date with the latest industry developments.

Medality’s flexible practice development platform includes more than 100 courses, 4,000 bite-sized microlearning videos, & over 4,000 integrated, scrollable cases designed to simulate a workstation.
Our case-based education is accredited under MRI Online by the Accreditation Council for Continuing Medical Education (ACCME) and totals more than 600 AMA PRA Category 1 Credits™ across the platform.
Courses are developed in partnership with hundreds of top academic faculty, such as:
Learners can earn unlimited CME & SA-CME credits across 135+ courses to meet their CME and certification requirements. Medality helps to fulfill:
Medality offers a wide range of CME courses, covering a variety of radiology subspecialties and modalities. Our courses and fellowships are designed to be engaging and interactive, allowing your radiologists to learn at their own pace and on their own schedule.
With Medality, you can say goodbye to spreadsheets and chasing your radiologists to complete or collect their certifications. Our platform offers completion tracking, so you can easily monitor your team’s progress and ensure that everyone is on track. You can also integrate our platform with credentialing software, making it even easier to manage your team’s certifications and licenses.
Learn how Medality can help you streamline the CME process for your radiologists.
If ever there was a case to be made for the importance of quality and patient care in radiology it is this one statistic: the real-time error rate in daily radiology practice is 3 to 5 percent, representing 40 million diagnostic errors annually worldwide.1 To make matters worse, the retrospective error rate in radiologic examinations is approximately 30 percent.2 In an environment where physicians are increasingly reliant on imaging for patient diagnosis and care plans, quality and patient care hang in the balance.
The good news is that diagnostic errors are preventable events, root causes can be readily identified, and real time solutions can be hardwired into department protocols and staff training.
However, administration must have the will, departments must have the budget, and staff must be engaged. Quality must be priority number one for every radiology department – and every radiologist.
As physicians and payers require more imaging to support diagnoses, radiologists are experiencing a steep workload with reduced support staff, rising quality expectations, and in some organizations, antiquated technology. This is increasing stress levels and burnout rates in radiologists, exacerbating an already risky environment with errors that occur all too frequently.
Medical errors and misreads can take different forms in radiology, including:
Several factors contribute to the occurrence of medical errors and misreads in radiology. Burnout, for example, can result in fatigue and decreased focus, leading to misreads or errors. Radiologists who specialize in a particular subspecialty or modality may not have enough exposure to other specialties, leading to potential errors when interpreting unfamiliar images. Additionally, staff members may be under pressure to read a high volume of imaging studies quickly, leading to errors or misreads.
Another contributing factor to misreads in radiology is the increasing demand for imaging studies. “The demand for imaging is outpacing what we’re doing on the training side,” said Dr. Vahid Yaghmai, professor and chair of radiological sciences at the University of California, Irvine. “The number of radiologists in the workforce is not growing as fast as the population and the demand for imaging.”3
There are not enough radiologists available to read these studies, and even if there are, they may not have the appropriate training in other subspecialties or modalities to handle the volume of imaging adequately. This situation can result in more misreads or errors due to the radiologist’s lack of experience.
Given the myriad issues resulting in misreads and errors, how can patient care be improved? The answer is a methodical approach that assesses and addresses each issue proactively, combined with an action plan for immediate assessment of issues in real time.
Here’s how to address the issues raised above:
The bottom line is that everyone in an institution bears the responsibility of protecting and improving patient care. When it comes to the radiology department, their specific efforts must be supported by quality and risk, finance and administration. Just as “no man is an island”, no department functions completely alone.
Radiology must have robust support in order to deliver highly accurate interpretations and improved reporting quality. That means:
It could be said that every patient diagnosis begins with imaging and the interpretation of those images are the first milestone in the patient care pathway. Therefore, this essential function must be supported with training, trust, and empowered radiologists that feel free to share concerns and seek advanced training. When these tools are placed in the hands of the experts in the department, errors can be addressed, quality will improve, and patient care will be enhanced.
[1] Radiographics https://pubs.rsna.org/doi/10.1148/rg.2018180021
[2] American Journal of Roentgenology https://www.ajronline.org/doi/full/10.2214/AJR.12.10375#:~:text=Every%20radiologist%20worries%20about%20missing%20a%20diagnosis%20or,claims%20against%20radiologists%20are%20related%20to%20diagnostic%20errors
[3] Radiological Society of North America https://www.rsna.org/news/2022/may/Global-Radiologist-Shortage
As a practice leader, it is your responsibility to ensure that your radiologists are meeting their CPD requirements. The Royal Australian and New Zealand College of Radiologists (RANZCR) have recently updated its CPD requirements to promote the continuous learning and development of radiologists, ensuring that they remain up-to-date with the latest advancements and technologies in the field of radiology. The new requirements focus on promoting evidence-based practice and encourage radiologists to reflect on their professional practice and engage in continuous improvement.
These updated guidelines were developed to better align with the requirements of the Medical Board of Australia (MBA), and the Medical Council of New Zealand (MCNZ) and to provide radiologists with a more flexible and personalized approach to professional development. This change brings new opportunities for professional growth, but it also means that radiologists will require guidance and support to navigate the new requirements.
The new CPD program requires radiologists to:
There will also be an additional minimum requirement of activity that needs to be met across the 3 broad categories:
1. Compliance
Radiologists must comply with the new RANZCR CPD requirements, which means that they must complete a certain number of CPD activities each year. Practice leaders must ensure that their radiologists are aware of the updated requirements and are meeting them.
2. Professional Growth
The updated RANZCR CPD program offers radiologists more opportunities for professional growth, including a greater focus on reflective practice and self-directed learning. Practice leaders must help their radiologists to take advantage of these opportunities and provide support for their ongoing development.
3. Improved Patient Care
By meeting the updated RANZCR CPD requirements, radiologists can enhance their knowledge and skills, which will ultimately lead to improved patient care. Practice leaders must recognize the importance of this and encourage their radiologists to embrace the updated program.
4. Competitive Advantage
Practices that have radiologists who are meeting the updated RANZCR CPD requirements will have a competitive advantage in the marketplace. Patients and referring doctors are likely to prefer practices with radiologists who are committed to ongoing professional development.
5. Reputation
A practice’s reputation is closely linked to the reputation of its radiologists. By helping their radiologists to meet the updated RANZCR CPD requirements, practice leaders can enhance their practice’s reputation as a center of excellence in radiology.
Practice leaders have a critical role to play in ensuring that their radiologists meet the updated RANZCR CPD requirements. By providing guidance and support, practice leaders can help their radiologists to embrace the new opportunities for professional growth and ultimately deliver better patient care.

Find the 2023 RANZCR CPD requirements here.
It is no secret that radiologists are leaving their jobs. In fact, over 41% of radiologists changed their jobs over a 4-year period, according to a recent study.1 The study included 25,228 radiologists who were associated with 4,381 practice groups across the country. Practice separation rates were 47% for multi-specialist groups as opposed to 38% for radiology-only practices.
Burnout, workload, and inability to participate in nonclinical work, such as professional development and practice building, are the primary drivers.2 But the demand for radiology and medical imaging has only increased in our post-COVID world.
Even with this uptick in demand, radiologists still say they need to focus more on nonclinical work to improve their accuracy and outcomes. In fact, 56.9% of respondents indicated that they made reading errors because they were rushed by increased workloads. This situation hurts providers and patients alike.
But what about the impact of these trends on practices and their leaders? A critical, but under-discussed, downstream impact of the Great Radiology Resignation is the impact it has on practices and practice leaders.
Practice leaders are scrambling to protect their precious workforce. Radiology’s resignation trends are having a major impact, not just on individuals and patients, but also on practices and their leadership. But it is not too late.
The way a practice leader recruits and trains radiologists affects the entire practice – not just the radiologist. There are two primary downstream impacts when practices invest in their radiologists:
At the individual level, the retention of highly-trained radiologists is a good thing for the practice overall. Good retention rates can indicate radiologists are happy, they are not burnt out, and they are working productively and efficiently. More radiologists staying in their roles also means that overall morale and camaraderie are likely to be high.3
One bonafide path to improving retention and morale is to invest in radiologists’ training and professional development. By investing in radiologists’ training, practice group leaders send a message that they care about their providers’ growth, well-being, and commitment to the field. This investment improves specialty range, recruitment, and coverage.
Because of lack of supply and increased demand, radiologists in private practices must be able to pivot and read outside of their specialties. Practices no longer have the luxury of remaining siloed by specialty. This can actually benefit leaders.
With proper investment in professional development and training, especially through innovative avenues like microlearning, practice leaders can develop a nimble workforce with confidence and competence. This results in expanded practice capabilities, quicker turnaround times, and a wider breadth of offerings.
For example, a practice that may have been limited to one or two specialties, now could offer cardiac CT or breast imaging, when that practice may not have been able to before. This also means that practices may be able to solicit business from a wider range of hospitals, clinics, and outpatient centers.
Radiology business leaders try to entice highly-skilled radiologists with bonuses, extra vacation time, and wellness perks. While these tools may work in the short-term, radiologists want to work in a place where they feel that their leaders care about their growth, well-being, and satisfaction.
The most obvious and effective way to retain radiologists long-term is to offer consistent and ongoing access to training and professional development, especially in innovative ways. This approach is, often, more cost-effective for practices than ever-increasing bonuses, increased salaries and paid time off. When practice leaders invest in their providers, word spreads and the reputation of the practice grows. Over time, this allows the practice to organically attract and retain excellent providers.
The available literature about radiologist burnout, retention, recruitment, and resignation focuses almost entirely on the impacts of these challenges on individuals. However, it is time for the imaging community, especially practice leaders and business managers, to understand the market and economic landscape, focus on the impact it has on their practices and proactively develop solutions so they can continue to grow.
[1] https://www.neimanhpi.org/press-releases/radiologists-job-changes-trends/
[2] https://healthimaging.com/topics/medical-imaging/neuroimaging/burnout-369-radiologists-early-retirement
[3] https://projectionsinc.com/abetterleader/morale-the-number-one-factor-for-employee-retention-and-productivity/
Very few radiologists work exclusively in siloed subspecialties. As other areas of medicine specialize and subspecialize, it becomes increasingly important for radiologists to increase their range and grow more nimble across many specialties. Dr. David Youmans of Princeton Radiology Associates says that “multispecialty radiologists are…likely to become even more valuable as more referrals originate from less rigorously trained providers.”
Historically, a generalist was defined as a non-fellowship trained radiologist. This is no longer the case. Now, a generalist is “a practitioner for whom no single specialty represents a majority of their billed relative value units (RVU’s).”1
Over 55% practicing radiologists meet the definition of a radiology generalist. However, the term “general radiologist” may be antiquated. This is because, among general radiologists, over 85% of them derive their billable work from two or more distinct subspecialty areas.
Multispecialists are the way of the future. About 98% of radiologists are fellowship trained. Because of the trend towards multispecialists, most radiology programs offer 4-6 month mini-fellowships in the 4th year of residency. This illustrates academic centers’ recognition that a single fellowship is, likely, not enough for today’s radiologist to succeed. This shift towards multispecialists may be especially important in rural and underserved areas because multispecialty radiologists can cover many different types of common exams and lower complexity procedures.
A number of factors contributed to the increase in multispeciality radiologists.
Workload and volume have massively increased, resulting in massive shortages nationwide for mammographers, pediatric radiologists, cardiothoracic radiologists and more. To keep up with volumes, radiologists have to practice beyond their core specialty because hiring additional FTE and even outsourcing is no longer viable.
After a decades-long focus on increasing subspecialization, many of today’s radiologists are caught off-guard by the need to be a multi-specialist. That is why we must now undertake two changes:
In 2020, the American College of Radiology passed Resolution 47. Resolution 47 established a taskforce to explore the concept of the “Multispecialty Radiologist.” The taskforce discovered that radiologists do not care about the title of multispecialty radiologist, nor do they agree upon an exact definition.2 That said, there is no debate as to whether there is an ever increasing trend towards radiologists as jacks-of-all-trades. As a result, it is imperative that the broader radiology community embrace this concept and all of the doctors who fall into this category.
Once that occurs, the next thing that has to happen to curtail massive burnout, resignation, and discontent among radiologists today is to support this new reality. To do this, we must maximally equip multispecialty radiologists with the tools that they need to be confident, competent, and efficient reading across specialties. Because this is a shift in how we think about radiologists and their training needs, an appropriate shift in how we train and equip them needs to follow suit.
This shift cannot be slow. We need to invest now in new and innovative ways of training radiologists so that they can read across specialties. These investments include digital microlearning, peer-to-peer mentoring, classic CME across a range of subspecialties, and conference opportunities. When this happens radiologists reading across specialties will become more facile, confident, and competent. The downstream impacts of this will be at the practice level. As more radiologists become more competent and confident, more practices will become more profitable, nimble, and successful at retaining and recruiting top talent.
[1] https://vulcanimaging.com/wp-content/uploads/2021/08/Value-of-the-New-General-Radiologist-in-Private-Practice.pdf
[2] The definition used in this document is one of many others. The author feels that this definition accurately describes the concept being discussed.
Radiology may be the only medical subspecialty that touches every other subspecialty. This means that radiologists are critically important for a properly functioning medical system. But, increasingly, radiology practice managers and leaders are facing unprecedented and magnified problems. If they do not find solid solutions, all of medicine will suffer. Practice managers are battling retention, recruitment, burnout, and workload challenges to ensure that their quality and revenue remain high. Each of these challenges comes with its own nuance and needs.
The majority of radiology practice managers cite staffing levels as their biggest and most pressing challenge.[1] There is a national shortage of radiologists. A 2020 Journal of the American College of Radiology (JACR) study indicated that in the preceding 4-year period (2014-2018), practice separation rates increased by 38% and 41% of all radiologists left their jobs in that same period.[2] Early-career, late-career, and general radiologists were most likely to leave their jobs. This was all before COVID. In fact, a major 2017 survey in the European Journal of Radiology indicated that 36.9% of neuroradiologists contemplate early retirement. Burnout, workload, and inability to participate in non-clinical work, such as professional development, and practice building are the primary drivers of this burnout and resignation. In addition to a desire to focus more on nonclinical work, 56.9% of respondents indicated that they made reading errors because they were rushed by increased workloads. These errors impact provider confidence and competence, as well as patient safety.
The nature of radiology has changed. COVID-19 accelerated changes that were slowly creeping into the profession. Now, radiologists are often likened to emergency medicine doctors. This is because they are expected to be available 24/7 to read films from ER’s fielding more workload than ever. This is especially true for safety-net hospitals where the majority of patients often originate from the ER. There are two major downstream consequences to ER and remote demands dominating many private and academic radiology practices.
These demands are causing many radiologists to throw up their hands and quit, leaving practice managers with huge staffing shortages.
Prior to COVID, it was obvious that radiology practice leaders and chairpersons needed short term wins and longer term goals to be successful. COVID forced these leaders to live in fight-or-flight mode to survive two years of economic uncertainty, patient volume variation, staffing challenges, and enormous stress. Anyone who lived through COVID cannot say with full confidence that things will be more steady but, it appears that radiology patient loads will return to 2019 levels.[1] This means that it is time for leaders to plan for the long game.
The best way to do this is to invest in good people. Practice leaders inherently understand that investing in their doctors leads to greater growth, revenue, retention, and recruitment. However, this intuition was abandoned during COVID when practice leaders lived on a razor’s edge at every moment. Now is the time to resort back – to invest in the long term in good doctors, leaders must understand what they need and stay up with the times. To do this, practice leaders must understand the root causes of retention and recruitment challenges. The primary cause today is burnout.
Physicians, especially radiologists, are suffering from real and serious burnout. A medscape survey revealed that 49% of radiologists report feeling burnt out[1] and 54-72 percent have symptoms of burnout. The reasons for this burnout are multifactorial.
Work-life balance, or lack thereof, is a major driver of this epidemic in radiology. Of the radiologists who feel burnt out, 50% attribute that burnout to a lack of control or autonomy.[1] In fact, 62% of radiologists polled said they would be willing to reduce their pay in exchange for better life-work balance.[2] Dr. Richard Duszak, Chair of Radiology at the University of Mississippi, said that CME accreditation requirements are serious contributors to burnout for radiologists today.[3] Young parents and women, in particular, are hard hit by work-life balance struggles in radiology.
A recent American Medical Association survey reported that 92% physicians under age 35 felt that work-life balance is important, but only 65% felt that they had achieved this goal.[4] Radiology is especially hard-hit. While the number of women enrolled in medical schools exceeded that of men in 2017, only about 27% of radiologists are women.[5] In the previously cited Medscape survey, only 44% of men reported feeling burnt out as compared with 65% of women.[6] All of these statistics indicate the need for radiology practice managers to take burnout very seriously, especially among younger and female faculty.
In Minneapolis, radiology giant, vRad, recently partnered with Vital WorkLife, a behavioral health consultancy, to address burnout among its radiologists.[7] Vital WorkLife found that two of the top drivers for burnout and dissatisfaction among radiologists at vRad are inflexible schedules and work-life imbalances.
What radiologists need is fulfillment, flexibility, and motivation. Once practice leaders understand the root causes of radiologist burnout and defection, they can implement solutions that work. Practice managers must, first and foremost, recognize that radiologists are humans. This may seem painfully obvious, but it merits mentioning. By understanding that radiologists are eager to learn, want to feel fulfilled, and need to be appreciated, practice managers can start to make changes that will curtail the great radiology resignation. By investing in radiologists’ professional development, growth, and overall success, practice managers can buck the trend of burnout and resignation and reignite their workforce with enthusiasm, energy, and commitment. Further, by investing in these elements now, practice managers can generate a reputation that attracts new talent to increase revenue and production. Today’s radiologist is often expected to be a renaissance person.
Practice managers should, therefore, create opportunities to upskill in high-growth, high demand areas rather than letting radiologists figure out how to navigate this landscape on their own.
In addition to classic professional development and medical education, it is prudent for practice managers to think innovatively about new and different ways to increase competence, happiness, and productivity in radiologists. Today, people – including doctors – are accustomed to having what they need at their fingertips. This is true of food, rides, exercise, and entertainment. Virtually everything can be delivered, streamed, or brought to people’s homes. This is yet to be true of medical education and professional development for radiologists. But that is about to change.
In addition to general investment in radiologists’ wellbeing and development, proactive leaders could set themselves apart by investing in the newest and best technologies to bring tech-based, innovative opportunities to advance radiology careers to their doctors. Microlearning is a great example of how this approach could create happier, more efficient doctors while generating more revenue and workplace satisfaction. This type of investment works for two reasons:
First, allowing doctors to learn and progress at their own pace, in their own place, and on their own schedules will offer the autonomy, trust, and flexibility that radiologists crave. Offering this as an option gives doctors a clear message that their leaders trust them, believe in their work, and care about their lives.
Second, giving doctors access to the world’s best faculty to better understand how to read challenging cases, especially those outside of their subspeciality of focus, opens a world to doctors to become more competent, confident, accurate, and efficient. By learning and growing in their field, doctors will feel as though they are valued and respected. This is especially important in recruiting and retention.
Like burnout itself, the antidotes to the problem are multifactorial and complicated. Practice managers must be innovative and nimble when addressing burnout. While solving this problem, practice managers, no doubt, also consider revenue and RVU’s and productivity. There is a shortage of radiologists so giving more of them time off helps the individuals but may hurt the practice.
Radiology leaders are pushing back. As Dr. Michael Recht, Chair at NYU Langone Medical Center emphasizes “we can’t tell everyone just to do clinical work. Radiologists need to take the time to talk to their referring physicians, to go to interdisciplinary conferences, and fulfill their educational mission.” When leaders ask radiologists just to increase clinical workload, radiologists leave. It’s that simple. Today’s radiology leaders must understand that there is a long game for success.
That is why it is time to figure out how to give radiologists more autonomy, more work-life balance and more satisfaction at work. A recent poll indicated that 60% of burnt out radiologists attributed those feelings to a lack of respect. When leaders invest in radiologists’ professional development, those leaders make it clear that doctors’ skills growth, pride, and confidence in their work – rather than just in RVU’s – matter.
Investing in professional development and innovative ways to increase fulfillment, autonomy, and trust will not solve all of practice leaders’ challenges in a post-COVD world, but it is a strong step in the right direction. This investment, among others, will allow leaders to remove some of the yoke imposed by COVID to plan for the future, attract and retain the best and brightest, and succeed in increasing revenue and improving patient care.
[1] https://radiologybusiness.com/topics/healthcare-management/radiologist-salary/dramatic-shift-new-survey-highlights-salaries-and
[2] https://www.neimanhpi.org/press-releases/radiologists-job-changes-trends/#:~:text=Researchers%20found%20that%20over%20the,job%20during%20the%20study%20period.
[3] https://healthimaging.com/topics/medical-imaging/neuroimaging/burnout-369-radiologists-early-retirement
[4] https://www.appliedradiology.com/articles/coping-with-covid-resilience-in-radiology
[5] https://radiologybusiness.com/topics/healthcare-management/leadership/radiologists-burn-out-medscape-radiology-physician
[6] https://radiologybusiness.com/topics/healthcare-management/leadership/radiologists-burn-out-medscape-radiology-physician
[7] https://www.diagnosticimaging.com/view/has-burnout-become-an-epidemic-in-radiology-
[8] Id.
[9] https://www.healthecareers.com/articles/career/millennial-physicians-setting-healthier-work-life-balance
[10] https://dailybulletin.rsna.org/dailybulletin/index.cfm?pg=20mon06
[11] https://radiologybusiness.com/topics/healthcare-management/leadership/radiologists-burn-out-medscape-radiology-physician
[12] https://www.prnewswire.com/news-releases/vrad-selects-vital-worklife-to-support-its-national-remote-workforce-301646288.html